Basketball is a sport defined by speed, power, and agility. These athletic qualities, while essential for performance, place extreme mechanical demands on the human body—particularly the ankle and foot. As such, it’s no surprise that professional basketball players suffer a disproportionately high rate of Achilles tendon (AT) ruptures, a devastating injury with profound implications for career longevity and post-injury performance.
Much of the conversation around Achilles injuries focuses on the calf muscles—the gastrocnemius, soleus, and plantaris. While these three muscles form the structural foundation of the Achilles tendon, this narrow focus ignores the broader neuromuscular system responsible for force generation and control around the ankle and foot. To truly understand both the mechanism of injury and the path to prevention, we must look beyond the obvious.
The ankle is stabilized and moved not just by the superficial calf muscles, but by an entire network of extrinsic and intrinsic musculature working in unison. Muscles like the tibialis anterior, fibularis longus and brevis, extensor digitorum longus, flexor hallucis longus, and tibialis posterior all contribute significantly to the regulation of ankle motion through dorsiflexion, plantarflexion, inversion, and eversion. These muscles originate in the lower leg and cross the ankle joint to insert into various regions of the foot, collectively controlling not only movement, but load distribution and stability during every step, jump, or cut.
Within the foot itself lies a sophisticated array of intrinsic muscles, many of which are often overlooked in both training and rehabilitation. These include the abductor hallucis, flexor digitorum brevis, adductor hallucis, interossei, and lumbricals, among others. Though small in size, these muscles are critical for maintaining the structural integrity of the foot, particularly the medial and transverse arches. Their ability to generate isometric force under load determines whether the foot can remain rigid during propulsion and absorb shock during landings.
Despite the complexity of this muscular system, many training programs focus disproportionately on dynamic movement and isolated mobility drills, often without developing the athlete’s ability to tolerate or generate isometric force in these newly accessible positions. This is especially dangerous when increasing ankle dorsiflexion range of motion. While enhanced dorsiflexion is commonly seen as beneficial, if an athlete cannot produce and tolerate game-forces at these expanded ranges, they enter a biomechanical danger zone.
This danger is most clearly seen in the mechanism of Achilles tendon rupture—particularly the false-step. This injury mechanism frequently involves a backward step with the injured leg landing outside the body’s center of mass, with no forward translation. This places the ankle in a highly compromised position. As the athlete attempts to decelerate or change direction, the injured foot strikes the ground behind the body while the trunk lowers and the ankle rapidly dorsiflexes. In this moment, the musculotendinous system must absorb massive ground reaction forces while transitioning the body in a new direction.
And here's the key point: this transitional phase between dorsi flexion and plantar flexion—regardless of how brief—is instantaneously isometric in nature. The body must generate high levels of isometric force to arrest momentum and redirect it. If the athlete lacks sufficient isometric strength—not just in the triceps surae, but across the entire system supporting the ankle and foot—tissue strain or rupture becomes highly probable.
In vivo studies suggest that peak strain in the Achilles tendon ranges from 6.2% to 10.3% during high-intensity movements. However, observed failure points in cadaveric studies occur within a similar range. This implies that athletes operating at extreme end-ranges, especially under fatigue or high load, are working dangerously close to structural failure thresholds. In basketball, where ankle dorsiflexion has been shown to increase post-game, players may unknowingly place their tendons in even more vulnerable positions.
It’s not enough to simply gain more range. Athletes must be conditioned to generate, tolerate, and transfer force within that range. That means developing high-level isometric force capacity across every joint and segment contributing to ankle stability—from the hips and trunk down through the foot. When any part of this system is underprepared, the ankle and Achilles tendon often pay the price.
The prevention of Achilles tendon ruptures, therefore, requires a paradigm shift. We must stop thinking in isolation and start thinking in systems. A basketball athlete’s ability to withstand and respond to the forces of the game depends on the total sum of their isometric strength, not just their mobility or plyometric power.
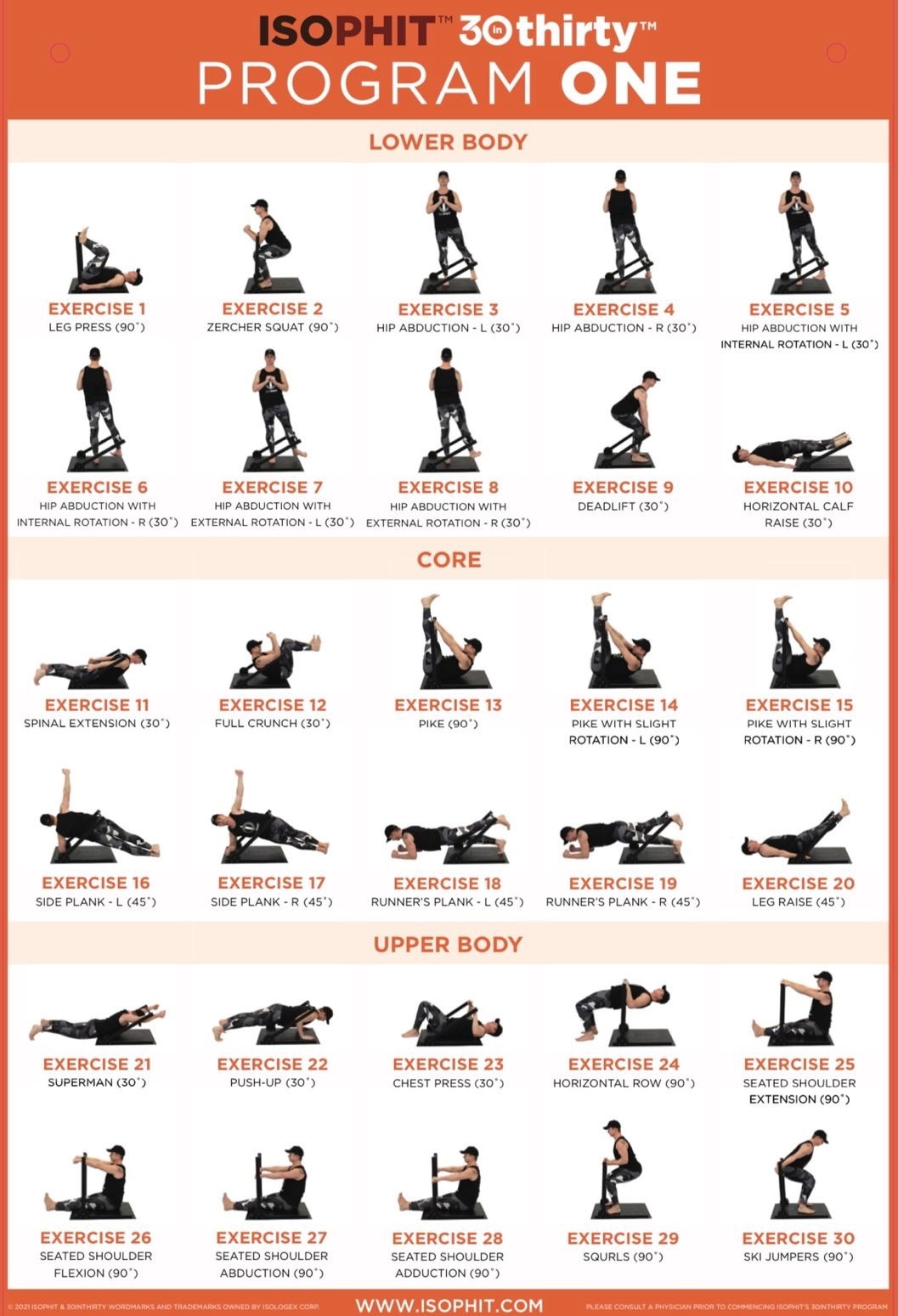
Tools like Isophit allow athletes and professionals to train every muscle involved in ankle and foot function—at every joint angle, and under controlled, consistent workloads. This helps athletes to build strength exactly where they need it most: in the high-risk, high-demand ranges where injuries occur.
In the end, the false-step that ends a season—or a career—isn’t caused by one bad movement. It’s the predictable result of an athlete being strong in some places, but weak where it matters most. By building isometric strength across the entire body, we give athletes the tools to not just move better—but to move safely and stay in the game.
For more insight into the false step mechanism read this: Mechanisms of Achilles Tendon Rupture in National Basketball Association Players
At Isophit, we help the world’s strongest, fastest, and most dominant athletes to win more, hurt less, and age stronger!
Join Team Isophit at www.isophit.com